Estimated Prevalence and Cost of Diabetes
|
Prevalence (1) |
2023 |
2033 |
|---|---|---|
|
Diabetes (type 1 + type 2 diagnosed + type 2 undiagnosed) |
104,000 / 19% |
124,000 / 22% |
|
Diabetes (type 1 and type 2 diagnosed) |
73,000 / 14% |
87,000 / 15% |
|
Diabetes (type 1) |
5-10% of diabetes prevalence |
|
|
Diabetes (type 1 + type 2 diagnosed + type 2 undiagnosed) and prediabetes (includes undiagnosed) |
192,000 / 36% |
217,000 / 39% |
|
Increase in diabetes (type 1 and type 2 diagnosed), 2023-2033 |
19% |
|
|
Direct cost to the health care system |
$72 million |
$81 million |
|
Out-of-pocket cost per year (2) |
||
|
Type 1 diabetes costs, % of family income |
$520-$9,169 / 2%-12% |
|
|
Type 2 diabetes costs, % of family income |
$401-$6,394 / 1%-9% |
|
Impact of Diabetes
- Among Newfoundlanders and Labradorians (1):
- 36% live with diabetes or prediabetes, and
- 14% live with diagnosed diabetes, a figure that climbs to 19% when cases of undiagnosed type 2 diabetes are included.
- Diabetes contributes to (5):
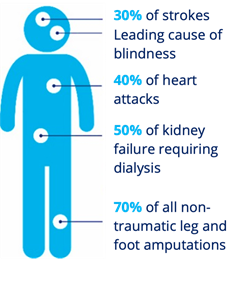
- Diabetes complications are associated with premature death (3). Diabetes can reduce lifespan by five to 15 years (3). It is estimated that the all-cause mortality rate among people living with diabetes is twice as high as the all-cause mortality rate for those without diabetes (4).
- People with diabetes are over three times more likely to be hospitalized with cardiovascular disease, 12 times more likely to be hospitalized with end-stage renal disease, and almost 20 times more likely to be hospitalized for a non-traumatic lower limb amputation compared to the general population (3).
- 33-50% of people living with diabetes experience diabetes distress (an overwhelming feeling about their condition that can lead to unhealthy habits like not checking their blood sugar or skipping medical appointments, etc.) (6).
- Individuals with depression have a 40% – 60% increased risk of developing type 2 diabetes (6).
- Diabetic retinopathy, a retinal vascular disorder that occurs as a complication of diabetes, is a leading cause of new cases of blindness in Canada, and often affects working-aged adults (7).
- Vision loss is associated with significant morbidity, including increased falls, hip fractures, and an increased risk of death (8).
- Foot ulceration affects an estimated 15-25% of people with diabetes in their lifetime (9).
- Compared to the general population, adults living with diabetes in Canada are over 20 times more likely to undergo non-traumatic lower limb amputations - 85% of which are preceded by foot ulcers (10).
- Hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) may affect mood and behaviour and can lead to emergency situations if left untreated (11).
- For people living with diabetes, adherence to treatment is affected by costs which are not covered by their public drugs and devices coverage (2).
- Those with type 1 diabetes can pay up to 12% of their gross annual income on medications and devices that range from $$520 to $9,169.
- Those living with type 2 diabetes can pay up to 9% of their gross annual income on medications and devices that range from $401 to $6,394.
Risk Factors for Diabetes
- The risk factors for type 1 diabetes are not well understood, but interaction between genetic and environmental factors are likely involved (11). Type 2 diabetes is caused by a combination of individual, social, environmental, and genetic factors (11).
- Certain populations are at higher risk of developing type 2 diabetes, such as those of African, Arab, Asian, Hispanic, Indigenous, or South Asian descent, those who are older, have a lower level of income or education, are physically inactive, or are living with overweight or obesity (11).
- The age-standardized prevalence rates for diabetes are 16% among people of South Asian descent, 13.3% among Black adults, 12.5% among people of Arab/West Asian descent, 8.8% among people of East/Southeast Asian descent, and 5.7% among people of Latin American descent (12).
- The prevalence of diabetes among First Nations adults living off reserve, Metis adults, and Inuit adults is 1.72 times,1.22 times, and 1.18 times higher respectively than the prevalence among non-Indigenous adult (12). In addition to the risk factors that impact all people in Canada, the ongoing burden of colonization continues to influence Indigenous peoples’ health.
- The prevalence of diabetes among adults in the lowest income groups is 2.1 times that of adults in the highest income group (12).
- Adults who have not completed high school have a diabetes prevalence 1.9 times that of adults with a university education (12).
- Social determinants of health can influence the rate of individual-level modifiable risk factors and thus the risk of diabetes. The main determinants of health include income, employment, education, childhood experiences, physical environments, social supports, access to health services, and racism (13).
Policy, Programs, and Services Related to Diabetes
- In Budget 2023, the government announced a CGM pilot project to evaluate the effectiveness and outcomes of this technology.
- On September 1st, 2022 the government implemented a sugar-sweetened beverage tax to address the impact of chronic disease, such as diabetes.
- In January 2021, the insulin pump program was expanded to include full coverage for eligible individuals with type 1 diabetes up to age 18 years, and full coverage for those 18 to 25 years for individuals already in the program. New clients to the program 18 years and older will be income tested to determine public coverage.
- The Newfoundland Project: Diabetes Canada, in partnership with eDOCSNL, the provincial electronic medical records (EMR) program, and Boehringer Ingelheim, launched a pilot project integrating Diabetes Canada’s Clinical Practice Guidelines with the EMRs being used by health-care providers in a diabetes collaborative in Corner Brook. Phase Two began in 2021.
- In May 2018, foot care for provincial Prescription Drug Program clients living with diabetes who also receive home support services was expanded to those who are over 65 years old.
- In June 2017, the government released its Chronic Disease Action Plan that included initiatives for diabetes.
- In 2014, the government released Guidelines for Diabetes Management in Schools.
Challenges
Newfoundland and Labrador faces unique challenges in preventing type 2 diabetes and meeting the needs of those living with diabetes:
- Non-modifiable risk factors of type 2 diabetes include age, gender, and ethnicity (11).
- The median age in Newfoundland and Labrador is 46 years (14). 19.4% of Newfoundlanders and Labradorians are over 65 years old (14). The risk of developing type 2 diabetes increases with age (11). Older adults living with diabetes are more likely to be frail and progressive frailty has been associated with reduced function and increased mortality (15).
- Adult men are more at risk of type 2 diabetes compared to adult women (11).
- Approximately 2.8% of Newfoundlanders self-identify as being of African, Arab, Asian, Hispanic, or South Asian descent (14). These groups are at increased risk of developing type 2 diabetes (11).
- There are 45,725 Indigenous people in Newfoundland and Labrador, who face significantly higher rates of diabetes and adverse health consequences than the overall population (16).
- Newfoundland and Labrador has high rates of individual-level modifiable risk factors (17):
- 49.7% of adults and 79.2% of youth aged 12 to17 are physically inactive;
- 34.4% of adults are living with overweight and 40.4% of adults are living with obesity;
- 80.6% of adults are not eating enough fruits and vegetables; and
- 22.3% of adults are current tobacco smokers.
- Factors related to the social determinants of health and that can influence the rate of individual-level modifiable risk factors among Newfoundlanders include income, education, food security, the built environment, social support, and access to health care (3).
- Newfoundland and Labrador has a rural population higher than the national average (18). For people with diabetes, accessing care is more challenging in rural areas across Canada than in urban areas.
- The median after-tax family income in Newfoundland and Labrador is among the lowest among the provinces (19).
Diabetes Canada’s Recommendations to the Government of Newfoundland and Labrador
- Fund a provincial diabetes framework
- Allocate funding to develop and implement a comprehensive diabetes framework with measurable goals for improving diabetes prevention, treatment and health outcomes for the province.
- Expand access: Put patients at the centre of policy decisions
-
Eliminate barriers, including age discrimination, to access evidence-based, personalized diabetes treatments, including diabetes medications, devices, and supplies.
-
Provide equitable access to continuous glucose monitoring systems (isCGM & rtCGM) according to Diabetes Canada’s reimbursement recommendations.
- Protect students with diabetes
- Implement a mandatory standard of care for students with diabetes that aligns with Diabetes Canada’s Guidelines for the Care of Students Living with Diabetes at School.
- Prevent amputations
- Implement health policies that support the prevention and management of diabetes foot complications and reduce the risk of lower limb amputations.
References
- Canadian Diabetes Cost Model. Ottawa: Diabetes Canada; 2016.
- Diabetes and Diabetes-Related Out-of-Pocket Costs: 2022 Update. Diabetes Canada; 2022.
- Diabetes in Canada: Facts and figures from a public health perspective [Internet]. Ottawa: Public Health Agency of Canada; 2011 p. 126. Available from: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres-2011/pdf/facts-figures-faits-chiffres-eng.pdf
- Public Health Agency of Canada. Twenty years of diabetes surveillance using the Canadian chronic disease surveillance system. [Internet]. 2019. Available from: http://publications.gc.ca/collections/collection_2019/aspc-phac/HP35-122-2019-eng.pdf
- Hux J, Booth J, Slaughter P, Laupacis A. Diabetes in Ontario: An ICES Practice Atlas [Internet]. Institute for Clinical Evaluative Sciences; 2003. Available from: https://www.ices.on.ca/Publications/Atlases-and-Reports/2003/Diabetes-in-Ontario
- Diabetes Canada Clinical Practice Guidelines Expert Committee, Robinson DJ, Coons M, Haensel H, Vallis M, Yale JF. Diabetes and Mental Health. Can J Diabetes. 2018 Apr;42 Suppl 1:S130–41.
- Flaxel, Christina J.; Adelman, Ron A.; Bailey, Steven T.; Fawzi, Amani; Lim, Jennifer I.; Vemulakonda, G. Atma; Ying, Gui-shuang. Ophthalmology (Rochester, Minn.), 2020, Vol.127 (1), p.P66-P145
- Vu, H. T., Keeffe, J. E., McCarty, C. A., & Taylor, H. R. (2005). Impact of unilateral and bilateral vision loss on quality of life. The British journal of ophthalmology, 89(3), 360–363. https://doi.org/10.1136/bjo.2004.047498
- Yazdanpanah, L., Shahbazian, H., Nazari, I., Arti, H. R., Ahmadi, F., Mohammadianinejad, S. E., Cheraghian, B., & Hesam, S. (2018). Incidence and Risk Factors of Diabetic Foot Ulcer: A Population-Based Diabetic Foot Cohort (ADFC Study)-Two-Year Follow-Up Study. International journal of endocrinology, 2018, 7631659. https://doi.org/10.1155/2018/7631659
- Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med. 2017 Jun 15;376(24):2367–75
- Diabetes Canada Clinical Practice Guidelines Expert Committee. Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes. 2018;42(Suppl 1):S1:S325.
- Public Health Agency of Canada. Pan-Canadian Health Inequalities Data Tool, 2022 Edition [Internet]. Available from: https://health-infobase.canada.ca/health-inequalities/data-tool/
- Prinjha S, Wicklow B, Nakhla M, Banerjee AT. Toward the Goal of Understanding and Tackling the Social Determinants of Diabetes. Can J Diabetes. 2022 Aug 1;46(6):549–50.
- Government of Canada SC. Census Profile, 2016 Census -Newfoundland and Labrador [Province] and Canada [Country] [Internet].
- Meneilly GS, Knip A, Miller DB, Sherifali D, Tessier D, Zahedi A. Diabetes in Older People. Can J Diabetes. 2018 Apr;42:S283–95.
- Aboriginal peoples in Canada: Key results from the 2016 Census [Internet]. Ottawa: Statistics Canada; 2017 Oct p. 11. Available from: https://www150.statcan.gc.ca/n1/en/daily-quotidien/171025/dq171025a-eng.pdf?st=krvs_yCt
- Canadian Risk Factor Atlas (CRFA), 2020 edition. Public Health Agency of Canada. Available at Public Health Infobase: https://health-infobase.canada.ca/crfa/
- Statistics Canada. Table 17-10-0118-01 Selected population characteristics, Canada, provinces and territories [Internet]. 2009. Available from: Selected population characteristics, Canada, provinces and territories
- Table 11-10-0190-01 Market income, government transfers, total income, income tax and after-tax income by economic family type [Internet]. Ottawa: Statistics Canada; 2019 Dec. Available from: https://doi.org/10.25318/1110019001-eng