Overview
Diabetes Canada Clinical Practice Guidelines Expert Committee
Paul Poirier MD, PhD, FRCPC, FCCS, FACC, FAHA, Olivier F. Bertrand MD, PhD, Jonathon Leipsic MD, FRCPC, G.B. John Mancini MD, FRCPC, FACP, Paolo Raggi MD, FACC, FAHA, FACP, FASNC, FSCCT, André Roussin MD, FRCPC
Anchored List of chapter sections
1. Key Messages
- Compared to people without diabetes, individuals with type 1 and type 2 diabetes (especially women) are at higher risk of developing heart disease, and at an earlier age. Unfortunately, a large proportion will have no symptoms before either a fatal or a nonfatal myocardial infarction (MI). Hence, it is desirable to identify people at high risk for cardiovascular events, especially people with unknown established severe coronary artery disease.
- In individuals at high risk of coronary artery disease (based on age, gender, description of chest pain, history of prior MI, abnormal resting electrocardiogram and presence of several other cardiovascular risk factors), exercise stress testing is useful for the assessment of prognosis.
- Exercise capacity is frequently impaired in people with diabetes due to the high prevalence of obesity, sedentary lifestyle, peripheral neuropathy (both sensory and motor) and unknown vascular disease. For those unable to perform an exercise test, imaging testing, such as pharmacologic, nuclear stress imaging, stress echocardiography, coronary artery calcium scoring or coronary computed tomography angiography may be required. Most imaging techniques have been shown to be useful in prospective study in order to identify people at higher risk. However, so far, there is no head-to-head study showing which one is most cost-effective.
2. Key Messages for People with Diabetes
- People with diabetes are at increased risk for developing heart disease, and often present at an earlier age than people without diabetes.
- Discuss with your health-care provider how to screen for heart disease.
3. Introduction
The majority (65% to 80%) of people with diabetes will die from heart disease (1,2). Compared to people without diabetes, people with diabetes (especially women) are at higher risk of developing atherosclerotic disease, and at an earlier age. A high proportion of deaths occur in people with diabetes with no prior signs or symptoms of cardiovascular disease (CVD). Furthermore, people with diabetes have a high prevalence of silent myocardial ischemia, and almost one-third of myocardial infarctions (MIs) occur without recognized or typical symptoms (silent MIs) (3). The goals of screening are to improve life expectancy and quality of life by preventing MI and heart failure through the early detection of significant CVD. The concept of coronary risk equivalency in people with type 2 diabetes has been challenged and a meta-analysis reported that this is not the case (4). Therefore, there is heterogeneity in the CVD risk of people with diabetes, which needs to be better defined clinically. For any degree of perfusion abnormality, people with diabetes had a much greater risk of cardiac events and death compared with people without diabetes (5). Similar findings have been reported for stress echocardiographic techniques (6) and electron-beam computed tomography studies (7).
In general, good clinical practice considers screening for any disease appropriate only when an effective treatment is available. Hence the underlying assumption of a study wishing to evaluate if screening for CVD is worthwhile in terms of survival, is that an effective treatment is available and the study design should reflect this by testing screening and treatment together. This is not the case looking at the literature of screening for coronary artery disease (CAD) in people with diabetes (8,9). On the other hand, The Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial (10) and the subsequent Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial (11) represent the landmark trials in the field of stable CAD treatment. Both studies found no benefits in terms of survival of revascularization (surgical or percutaneous) over medical therapy in stable people with documented coronary artery stenosis. Of note, participants with markedly positive stress test were excluded in COURAGE. The Does coronary Atherosclerosis Deserve to be Diagnosed earlY in Diabetic patients? (DADDY) study main finding reported that screening for CAD and revascularization did not affect the occurrence of a first cardiac event in people with diabetes (12). These results are in line with the Detection of Ischemia in Asymptomatic Diabetes (DIAD), COURAGE and BARI 2D studies and confirm that to date there is no proven indication, in daily practice, to search for ischemia in people with diabetes without symptoms. However, when one is clinically suspicious of the presence of CVD, different modalities can be used to assess the presence of CAD in people with diabetes.
Role of stress testing
Exercise stress testing is useful in people with diabetes at high risk of CAD for the assessment of prognosis and the identification of individuals who may benefit from coronary artery revascularization to improve long-term survival. The most predictive clinical observation for CAD in the person with or without diabetes is a history of chest pain or discomfort, but these features will be absent in a significant proportion (20% to 50%) of individuals with diabetes (13–19). Clinical findings, such as dyspnea on exertion, resting electrocardiogram (ECG) abnormalities or multiple CVD risk factors for atherosclerosis, may also indicate the presence of CAD. Recognition of such features is of clinical importance, as the outcome of CAD events is worse in people with diabetes when shortness of breath is the primary symptom (13).
The presence of CAD risk factors and resting ECG abnormalities identify people with diabetes at increased risk of important CAD burden and abnormal stress ECG or perfusion imaging results (20). A resting ECG at the time of diagnosis of diabetes also provides a baseline to which future ECGs can be compared. In people with diabetes considered to be at high risk for CAD, a repeat resting ECG may detect changes that result from silent MI and lead to earlier detection of critical CAD. There is evidence that early screening and intervention in people with diabetes and silent ischemia is beneficial and may improve long-term survival (16,21). Screening with exercise ECG stress testing will find 3-vessel CAD in 13% to 15% of those with abnormal stress test findings (22) and lead to angiography with revascularization in 1% to 3% of asymptomatic individuals (22–24). Similar findings were reported recently in The For Asymptomatic Obstructive Coronary Artery Disease Among High-Risk Diabetic Patients Using CT Angiography, Following Core 64: A Randomized Control Study (FACTOR-64) trial. It randomized 900 participants to coronary computerized tomography angiography (CTA) screening (n=452) or standard care (n=448). CTA showed no CAD in 31%, mild stenosis in 46%, moderate in 12% and severe stenosis in 11% of the participants. Although there was no significant reduction in CHD events in this 900-person study, the authors concluded that coronary CTA screening led to more aggressive risk factor modification in 70% of participants, including improvements in statin use and more serum lipids and systemic BP (25).
The Definition of Ischemia in Asymptomatic Diabetes (DIAD) study prospectively investigated the value of routine adenosine stress myocardial perfusion scanning in asymptomatic people with type 2 diabetes ≥55 years for the prevention of coronary events (19). The baseline study showed either perfusion defects or stress-induced ECG abnormalities in 22% of participants and large defects in 6%. In this study, multiple risk factors for CAD did not help identify people with positive functional tests for CAD. Of note, baseline ECG was normal in all participants. A substantial portion of the DIAD population was defined as having intermediate/high baseline CV risk. Nevertheless, their annual CV event rate was low and not altered by routine screening for inducible ischemia. Yet, a randomized pilot study on the impact of stress testing to screen for CAD in asymptomatic subjects with diabetes suggested a significant reduction in cardiac death and MI (26). Larger and adequately powered studies are necessary to support this provocative observation before clinical practice is changed. In the Basel Asymptomatic high-Risk Diabetics' Outcome Trial, almost one-quarter of the 400 asymptomatic participants with type 2 diabetes had silent myocardial ischemia, which was associated with a worse outcome (27). The yield of myocardial perfusion imaging can be improved by selecting a higher-risk group of people with diabetes with symptoms, peripheral vascular disease (PVD), chronic kidney disease (CKD), an abnormal ECG or a high coronary artery calcium (CAC) score (e.g. >400 Agatston score) (28). The choice of initial stress test should be based on evaluation of the resting ECG, the individual's ability to exercise, and local expertise and technology. Thus, the yield of stress testing in asymptomatic people with diabetes can be improved by selecting people based on the pre-test probability of CAD. The retrospective studies that showed a high prevalence of stress test abnormalities included people with abnormal ECGs (43% with Q waves) and vascular disease (28%) (28).
Data using diverse imaging technology have been reviewed and reported recently (28), but the additional benefit of imaging on prognosis and quality of life is not clear. Studies using coronary CTA in asymptomatic people with diabetes mostly concluded that these people have a high prevalence of coronary atherosclerosis and obstructive CAD, as well as a higher prevalence of plaques with features of instability compared with subjects without diabetes. Furthermore, it is important to emphasize that a normal ECG does not offer a long-term warranty from CVD events in people with type 2 diabetes. It is the same with stress echocardiography and myocardial perfusion imaging where no events were recorded in the first 2 years of follow up among people with a normal stress echocardiography or normal nuclear scan but significantly increased thereafter (6,28–30).
People with diabetes without evidence of CAD seen on computed tomography coronary angiography have an excellent prognosis, with no cardiac events at 62-month follow up. Thus, this imaging modality can be a useful tool to reassure people with diabetes with suspected CAD regarding their outcome, with a warranty period of at least 5 years in the presence of a normal result (5,31). Of note, coronary CTA is often performed in addition to a standard diagnostic work-up. This approach may be particularly useful in specific subsets of people with diabetes with unknown CAD and equivocal or uninterpretable stress tests or in case of a discrepancy between clinical presentation and stress test results. Owing to the high prevalence of CAD, the role of coronary imaging in people with diabetes may be not to document the presence of coronary atherosclerosis but rather to identify those people with more extensive disease vs. those without any atherosclerosis. Although CT coronary angiography is able to predict the prognosis of people with diabetes on the basis of the presence/extent of CAD and plaque type, coronary imaging by computed tomography coronary angiography is not, as in case of invasive angiography, able to predict which plaque may progress to destabilization and rupture, potentially causing a clinical event.
ECG abnormalities that limit the diagnostic accuracy of a stress ECG include resting ST depression (1 mm), left bundle branch block or right bundle branch block, an intraventricular conduction defect with QRS duration >120 ms, ventricular paced rhythm or pre-excitation. Individuals with these resting ECG findings should have a stress test with an imaging modality, such as scintigraphic myocardial perfusion imaging or echocardiography. The role of other imaging modalities (anatomical imaging), such as coronary CT, calcium score, etc., in comparison to functional imaging, needs to be determined in individuals with diabetes.
Exercise stress testing can identify people with diabetes with silent ischemia; however, whether at large exercise testing results in improved outcomes in people with diabetes has not been demonstrated. The strongest and most consistent prognostic marker identified during exercise ECG stress testing is the person's maximum exercise capacity (13). Although exercise capacity is decreased in individuals with diabetes (32–34), it is still of prognostic importance (13). Silent ischemia is most likely to occur in individuals with diabetes who are older (mean age 65 years) and have elevated total cholesterol and proteinuria (23).
An ECG with ST-T abnormalities at rest has been shown to be most predictive for silent ischemia (Odds Ratio 9.27, 95% CI 4.44–19.38) and was the only significant predictor of silent ischemia in women (23). The relevance of ST-T abnormalities as a predictive factor for silent ischemia emphasizes the importance of recording a resting ECG in most individuals with type 2 diabetes. An abnormal ECG may indicate the need for further investigations and result in the earlier detection and more aggressive management of CAD (23). An abnormal exercise ECG is associated with an annual CAD event rate of 2.1%, compared with 0.97% in subjects with normal exercise ECG (26).
Myocardial ischemia (whether silent or symptomatic) detected during exercise stress testing in individuals with diabetes is associated with poorer long-term survival compared to individuals without diabetes (16). Silent MI is common (40%) in older asymptomatic individuals with type 2 diabetes, but is more frequent (65%) in those with diabetes who also have microalbuminuria (35). People with diabetes and silent ischemia have an annual event rate for CAD of 6.2% (50% of events were new-onset angina and 50% were cardiac death or MIs) (36). Thus, silent MI is a prelude not only to symptomatic ischemia, but also to potentially fatal events. Also, it has been shown in a randomized trial in people with silent ischemia (the vast majority of whom did not have diabetes) that long-term anti-ischemic drug therapy (11 years follow up) reduces cardiac events (cardiac death, nonfatal MI, acute coronary syndrome or revascularization) with preservation of ejection fraction (37). In a retrospective study analyzing 14,849 consecutive people (3,654 with diabetes and 11,195 without diabetes) undergoing a combination of exercise stress and pharmacologic stress testing (combined protocol received intravenous dipyridamole [0.56 mg/kg] infusion over 4 minutes followed shortly by symptom-limited treadmill exercise), it was observed that, despite significant perfusion defects, people with diabetes who achieve ≥5 metabolic equivalents (METs) during exercise stress single-photon emission-computed tomography (SPECT) myocardial perfusion imaging (MPI) have significantly reduced risk for future cardiac events. People with diabetes who achieved a high workload (≥10 METS) had a low annualized event rate of 0.9% (38). The importance of low exercise capacity associated to worse CVD outcomes has been also observed in a smaller study (39).
Exercise capacity is frequently impaired in people with diabetes due to the high prevalence of obesity, sedentary lifestyle, peripheral neuropathy (both sensory and motor) and unknown vascular disease in this population. Individuals who cannot adequately exercise on a stress test have a poorer prognosis than those who can, regardless of the reason for this incapacity. Perfusion imaging also provides important prognostic information. Myocardial perfusion imaging has similar predictive value for cardiac death and nonfatal MI in individuals with diabetes as in those without diabetes (40). For those unable to perform an exercise ECG stress test, pharmacologic stress imaging, using dipyridamole, adenosine or dobutamine testing, is required. Stress echocardiography and stress nuclear imaging have similar values for cardiac events in the general population (41), but no comparative data are available for the person with diabetes. In a meta-analysis of perfusion imaging, an abnormal scan was predictive of future CAD events in subjects with and without diabetes. However, the cardiac event rate in individuals with diabetes was significantly greater than in those without diabetes (41). The choice of the optimal imaging modality to detect stress-induced MI is best determined by local availability and expertise.
The utility of newer CAD diagnostic modalities, such as coronary CTA, CAC scoring and cardiac magnetic resonance imaging, is currently unknown in terms of guiding management decisions in patients with type 2 diabetes (42). Coronary CTA has emerged as a noninvasive tool for the diagnosis of CAD that enables assessment of the vascular lumen together with the arterial wall. Multidetector coronary CTA allows assessment of coronary atherosclerosis at an earlier stage compared with imaging techniques that help evaluate myocardial perfusion. The long-term prognostic value of coronary CTA in a large population of people with diabetes without chest pain syndrome was investigated (43). Coronary CTA demonstrated a high prevalence of CAD (85%), mostly non-obstructive CAD (51%). People with events were more often classified in a higher CAC-risk category but coronary CTA performed better than the CAC-score regarding the events prediction (43).
Studies have demonstrated that increased CAC in persons with diabetes is associated with increased prevalence of ischemic events and mortality and is a better predictor than the Framingham risk score (28). Also, it was reported in 392 people with type 2 diabetes that the best predictors of progression were baseline CAC score, statin use and A1C >7.0% during follow up (44). Of importance, people with diabetes but with no CAC demonstrated a survival rate similar to that of people without diabetes and no detectable calcium (5,7).
4. Peripheral Vascular Disease
Palpation of peripheral pulses is a routine clinical examination recommended in people with type 2 diabetes, especially those with suspected peripheral arterial disease (PAD). The procedure is simple, rapid, noninvasive and inexpensive, but it has high interobserver variability, depending on foot anatomic variation, clinician experience and patient examination conditions (45,46). The examination of peripheral pulses also is hampered by the presence of medial arterial calcification, which is common in people with diabetes (47).
PAD is a common manifestation of atherosclerosis in type 2 diabetes. PAD is especially frequent in people with type 2 diabetes, with an approximately threefold increased risk compared with a population without diabetes (48). PAD mainly affects the infrapopliteal arteries and may induce more damage in small than in large vessels in people with type 2 diabetes (49,50). In the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) clinical trial, the incidence of PAD was comparable to the incidence of major coronary events and stroke and intensive glucose intervention did not influence the risk for major PAD in participants free from PAD at baseline (HR 0.96, 95% CI 0.82–1.12, p=0.62) (51). The risk for PAD was also similar in participants randomly assigned to active BP treatment compared with placebo (HR 1.08, p=0.36) and in those assigned to both intensive glucose control and active BP treatment compared with standard glycemic control and placebo (HR 1.03, p=0.77) (51).
The impact of previous microvascular and CV disease on the risk of major PAD was analyzed in 10,624 people with type 2 diabetes free from baseline major PAD in the ADVANCE trial. Microvascular disease, particularly macroalbuminuria and retinal photocoagulation therapy, strongly predicts major PAD in people with type 2 diabetes, but CVD does not (52). In ADVANCE, higher A1C and urinary albumin to creatinine ratio (ACR) levels, absence of dorsalis pedis and posterior tibial pulses, and current smoking history at baseline, higher systolic and lower diastolic BP, both with use of antihypertensive drugs, were all independently associated with the risk for major PAD (52). In the UK Prospective Diabetes Study (UKPDS), age, A1C, systolic BP, high density lipoprotein cholesterol (HDL-C), previous CV disease and current smoking were found to be independent risk factors for PAD (53). In the BARI 2D trial, age, female sex, black African origin, smoking, pulse pressure, A1C and ACR were independent risk factors for PAD (54,55). The incidence rate of PAD was 3.5 times higher in BARI 2D than in ADVANCE, which may be explained by differences in each study's inclusion criteria and the definitions of PAD outcomes.
From an ethnic viewpoint, there may be a lower prevalence of PAD in people with diabetes and CVD from South Asia compared with those of white European descent (52,56). Absent dorsalis pedis and/or posterior tibial pulses are independent predictors of major vascular outcomes in people with type 2 diabetes (57). Indeed, absent compared with present peripheral pulses (n=2218) were associated with increased 5-year risks for major CV events (HR 1.47, p<0.0001), MI (HR 1.45, p=0.003), stroke (HR 1.57, p=0.0003), CV death (HR 1.61, p<0.0001), heart failure (HR 1.49, p=0.0002), all-cause mortality (HR 1.48, p<0.0001), major microvascular events (HR 1.17, p=0.04), nephropathy (HR 1.24, p=0.04), ESRD or renal death (HR 2.04, p=0.02) and peripheral neuropathy (HR 1.13, p=0.0008) after multiple adjustment (57). Compared with the presence of all peripheral pulses, the absence of at least 1 peripheral pulse was significantly associated with a higher incidence of major CV events, nonfatal MI, nonfatal stroke, CV death, heart failure, all-cause mortality, major microvascular events, new or worsening nephropathy, ESRD or renal death, new or worsening peripheral neuropathy and all-cause hospitalization.
It is important to emphasize that compared with the ankle-brachial index or other noninvasive vascular methods, the pedal pulse examination has a weak performance for the diagnosis of PAD (58–60), especially the dorsalis pedis pulse, which may be absent in healthy subjects without PAD (61). A previous study estimated the sensitivity and specificity of an abnormal dorsalis pedis pulse for the detection of PAD at 50% and 73%, respectively, and at 71% and 91%, respectively, for an abnormal posterior tibial pulse (58). Other studies reported that the sensitivity and specificity of undetectable pedal pulses varied from 5% to 32% and 98% to 99%, respectively (59,60). Nevertheless, the absence of peripheral pulses has been shown to be a strong and independent predictor of risk for major outcomes, especially major CV events, CV and all-cause mortality, heart failure and renal events, in people with type 2 diabetes (57). This data should encourage the examination of peripheral pulses to improve the early detection and treatment of vascular complications in people with type 2 diabetes, especially in areas with limited access to specialized medical centres and technical resources. Therefore, these simple clinical indicators should be used to improve risk stratification and treatment of these people.
5. CVD in Type 1 Diabetes
Incidence and prevalence of CVD
CVD complications are important causes of morbidity and mortality among individuals with type 1 diabetes, which may have been under-recognized in the past. The presence of late gadolinium hyper-enhancement is a marker of prior MI in people with diabetes with unsuspected CAD. Late gadolinium hyper-enhancement was demonstrated in 4.3% of asymptomatic people with type 1 diabetes in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) trial (62). Reported prevalence rates of CVD in type 1 diabetes vary between 3% and 12.4% (63–65). It is important to emphasize that the CVD risk burden and profile of people with type 1 diabetes differs from type 2 diabetes. The Diabetes United Kingdom longitudinal cohort study, including more than 7,000 participants with type 1 diabetes, reported that type 1 diabetes is associated with markedly increased adjusted HR for major CAD events (median follow up of 4.7 years) in both men (HR 3.6) and women (HR 9.6). Of such, these risk increments are comparable to those observed in people with type 2 diabetes (65). Major CVD events occurred in type 1 diabetes on average 10 to 15 years earlier compared with matched controls without diabetes. The age-adjusted relative risk for CVD in type 1 diabetes is 10 times that of the general population (66–68). The Pittsburgh Epidemiology of Diabetes Complications (EDC) study demonstrated that the incidence of major CVD events in young adults with type 1 diabetes (age 28 to 38 years) was 0.98% per year (69) and was as high as 3% per year after age 55 years, making it the leading cause of death in that population (64,65,70). Gender and race/ethnicity are important features of increased risk of CVD; male gender and African Americans have higher rates of CVD compared to Europeans (69).
Difference from type 2 diabetes
CVD in type 1 diabetes differs from type 2 diabetes, not only in that it presents at a younger age, but also in relation to gender, silent presentation and disease severity (66,67). There is a high prevalence of silent CAD in young adults with type 1 diabetes, which may be related to cardiac autonomic neuropathy. Finally, the disease process seems to be more severe in type 1 diabetes. Compared with controls without diabetes, people with type 1 diabetes are more likely to have severe coronary stenoses, involvement of all 3 major coronary arteries and distal segment disease, resulting in major CV events with poor outcome and/or early development of heart failure (66,67).
CAD and cerebrovascular disease
CAD appears to be more common than stroke. The cumulative incidence of CAD ranges between 2.1% (64) and 19% (71)depending on the characteristics of the population studied. For the most part, studies report an incidence of around 15% (65,72,73). Mortality rates from CAD are reported between 6% and 8% (71,73), are likely higher in men than women (in contrast to type 2 diabetes) (74), and in those >40 years of age compared to those <40 years of age (74). Stroke is still an important outcome in type 1 diabetes; the cumulative incidence of stroke was 3.3% over 6 years among African Americans (66), 5.9% over 20 years in the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) (72), and 0.74% per year in the EURODIAB study (64). Also, prevalence of silent brain infarcts or leukoaraiosis is extremely high (34.5%) in type 1 diabetes (75).
Peripheral vascular disease
PVD is an important vascular complication of type 1 diabetes. Incidence rates of lower extremity amputation vary by age from 3.6 per 1,000 person-years among individuals 25 to 44 years of age to as high as 7.2% (76). By age 65, the cumulative probability of PVD is 11% in women and 20.7% in men (77). Compared to the general population, the rate of PVD among those with type 1 diabetes may be very high (77). If one considers ankle-brachial index (ABI) <0.9 as the criterion for the presence of peripheral atherosclerotic disease instead of overt clinical events, 45.6% of participants from DCCT/EDIC study developed PVD (78). Predictors of PVD include increasing age, male gender, history of sores or ulcers, diastolic blood pressure, LDL-C, A1C, diabetes duration, hypertension, albumin excretion rate, glomerular filtration rate, smoking and retinopathy (76,78,79). In addition to the clinical endpoints of CAD, stroke and PVD, subclinical carotid disease may be commonly associated with type 1 diabetes. Compared to age-/sex-matched healthy controls, greater carotid intima-media thickness (IMT) has been observed in studies of children with type 1 diabetes with a mean age as young as 11 years (80–83).
Time course of events
Although CAD rarely presents within the first 20 years of diagnosis, by age 30 years, many individuals will have had type 1 diabetes for 20 years and rates of CVD begin to approach the high-risk category (84). The recent decline in CKD in diabetes has not been accompanied by a corresponding fall in CAD rates. Indeed, no temporal decline was noted for the cumulative incidence of MI/CAD death at 20, 25, or 30 years' duration of diabetes in the Pittsburgh EDC, despite at least a 50% decrement of the cumulative incidence of overt nephropathy (69). In fact, nephropathy or microalbuminuria no longer precedes CAD in the majority of cases. In the EDC study, there was no difference in the cumulative incidence of CAD stratified according to year of diagnosis (1950–1980), despite substantial declines in renal failure, as well as decline in overall mortality over the same time period (69). The DCCT intensive therapy intervention had a significant impact on the age and the duration of diabetes exposure at onset of CVD, despite the fact that no overt CVD was apparent at baseline (85). Thus, despite the well-recognized increase in CVD risk associated with proteinuria, it clearly explains only a portion of the CVD risk. In the DCCT study, the treatment group effect of intensive treatment therapy on CVD risk persisted after adjustment for microalbuminuria (HR 0.62) and albuminuria (HR 0.58), suggesting that, although diabetic kidney disease is important, differences in mean A1C are clearly significant drivers (85). In the same way, only 15% of the Oslo Study population had microalbuminuria, despite the fact that all participants had at least subclinical CAD (86). In the Pittsburgh EDC study, myocardial ischemia by ECG, as the initial manifestation of CAD, was less common and a documented MI was more common in those with prior renal disease compared to those without (87).
Effect of sex
Compared to women without diabetes, women with type 1 diabetes had a 3.5 times higher risk of having coronary artery calcification (88). While standardized mortality rates from ischemic heart disease were higher in men than women at all ages in the general population, there was no difference in mortality from ischemic heart disease in men and women with type 1 diabetes <40 years of age (74). Men with type 1 diabetes ≥40 years had a higher mortality rate from CVD than women with type 1 diabetes (89) in contrast to type 2 diabetes. In a large Norwegian cohort study, mortality rates from ischemic heart disease were higher in women with type 1 diabetes than in men or women without diabetes. However, men with type 1 diabetes had higher mortality rates than women with type 1 diabetes (90). A population-based cohort study showed different results (91). This study found that among those with type 1 diabetes, women had a 2.5 to 3 times higher standardized mortality rate from CVD than men with type 1 diabetes. Although not all the findings are consistent, the common thread in all these studies is that the presence of type 1 diabetes (as well as in type 2 diabetes) seems to dramatically increase the risk for CVD, particularly in women.
Testing for CVD in type 1 diabetes
In the absence of data to the contrary, one approach to identifying CVD in people with type 1 diabetes is to apply the same CAD risk assessment and diagnostic strategies used in type 2 diabetes (see discussion above) or in the population in general (92). This, however, does not support routine CAD screening beyond resting ECGs in people with diabetes who do not have CV symptoms or an abnormal ECG, favouring instead global CVD risk factor assessment and management.
People with type 1 diabetes who have symptoms suggestive of CAD, an abnormal resting ECG or clustering of CVD risk factors yielding an intermediate or high global risk estimate, acknowledging that risk scores are more or less accurate in type 1 diabetes, should have additional testing for CAD (92,93). For people able to walk on a treadmill without significant baseline ST segment abnormality (see discussion for type 2 diabetes), exercise treadmill testing remains the first-line diagnostic test due to the high cost efficacy and widespread availability. However, treadmill testing may not be possible due to the burden of peripheral neuropathy, foot pathology, lower extremity amputation and ECG abnormalities as left ventricular hypertrophy in the patient population with type 1 diabetes. Pharmacological stress imaging studies, such as nuclear myocardial perfusion imaging or pharmacological stress echocardiography may be required. Sophisticated testing has been reported in people with type 1 diabetes. CAC, assessed by CT imaging, is common (94,95) and more frequent in people with type 1 diabetes than in those without. In the Coronary Artery Calcification in Type 1 Diabetes (CACTI) study, 656 adult participants with type 1 diabetes showed a higher prevalence and extent of CAC than 764 age- and sex-matched control subjects with no difference between sexes (96). Progression of CAC is reduced by intensive glycemic control (95). The presence of CAC is independently associated with increased prevalence of CAD, even after adjustment for traditional risk factors (94), and test performance in people with type 1 diabetes is comparable to that of the general population.
In the Pittsburgh EDC longitudinal study, 302 adults with type 1 diabetes, with a mean age of 38 years, underwent CAC screening. The prevalence of CAC was 11% in participants <30 years of age and as high as 88% among those 50 to 55 years. CAC was independently associated with prevalent CAD across the entire cohort, with a stronger graded association in men than in women. While CAC assessment has proven to predict subsequent CV risk in the general population and in cohorts of people with type 2 diabetes (7), no data are yet available to determine the utility of CAC assessment for risk prediction in type 1 diabetes. Women with type 1 diabetes had just as much CAC as men; women without diabetes have less CAC than men (88).
In summary, asymptomatic people with diabetes are considered to be in a high global CAD risk, for which exercise ECG is rated appropriate and cardiac imaging techniques (stress radionuclide imaging, stress echocardiography, stress cardiac magnetic resonance, calcium scoring and coronary CTA) are all given a “may be appropriate” rating. This publication (97)emphasizes the concept that just because a test is rated “appropriate” or “may be appropriate,” does not mean that it must always be performed, and clinical judgment of the health-care professional always has its place (28). In asymptomatic people with diabetes without any previous cardiac event, screening for silent myocardial ischemia targeted to revascularization, has not been shown to provide benefits in terms of cardiac prevention. Widespread use of screening tests is not justified since it does not prevent first cardiac event (98). Thus, testing for the presence of CAD may modulate medical treatment (more aggressive risk factor management) but revascularization therapy has not been shown to alter outcomes in the asymptomatic person with type 2 diabetes except in people with decreased left ventricular ejection fraction but viable myocardium.
6. Author Disclosures
Dr. Leipsic reports personal fees from Heartflow and GE Healthcare, outside the submitted work. No other authors have anything to disclose.
Resources
Recommendations
- A resting ECG, repeated every 3 to 5 years, should be performed in individuals with diabetes with any of the following [Grade D, Consensus for all of the following]:
- Age >40 years
- Duration of diabetes >15 years and age >30 years
- End organ damage (microvascular, CV)
- ≥1 CVD risk factor(s) (current smoking, hypertension, family history of premature CVD in first degree relative [men <55 years, women <65 years], CKD, obesity [BMI >30 kg/m2], erectile dysfunction)
- Age >40 years and planning to undertake very vigorous or prolonged exercise, such as competitive running, long-distance running, or high-intensity interval training (see Physical Activity and Diabetes chapter, p. S54).
- People with diabetes should undergo investigation for CAD by exercise ECG stress testing as the initial test in the presence of any of the following:
- Typical or atypical cardiac symptoms (e.g. unexplained dyspnea, chest discomfort) [Grade C, Level 3 (13)]
- Signs or symptoms of associated diseases
- PAD (abnormal ankle-brachial index) [Grade D, Level 4 (18)]
- Carotid bruits [Grade D, Consensus]
- Transient ischemic attack [Grade D, Consensus]
- Stroke [Grade D, Consensus]
- Resting abnormalities on ECG (e.g. Q waves) [Grade D, Consensus]
- CAC score >400 Agatston score [Grade D, Consensus].
- Pharmacological stress echocardiography or nuclear imaging should be used in individuals with diabetes in whom resting ECG abnormalities preclude the use of exercise ECG stress testing (e.g. left bundle branch block or ST-T abnormalities) [Grade D, Consensus]. In addition, individuals who require stress testing and are unable to exercise should undergo pharmacological stress echocardiography or nuclear imaging [Grade C, Level 3 (40)].
- Individuals with diabetes who demonstrate ischemia at low exercise capacity (<5 METs) on stress testing should be referred to a cardiac specialist [Grade D, Consensus].
Abbreviations:
A1C, glycated hemoglobin; ACR; albumin to creatinine ratio; CAC, coronary artery calcium; CAD, coronary artery disease; CHD, coronary heart disease; CI, confidence interval; CKD, chronic kidney disease; CT; computed tomography; CTA, computed tomography angiography; CV, cardiovascular; CVD, cardiovascular disease; ECG, electrocardiogram, HDL-C, high density lipoprotein cholesterol; HR, hazard ratio; LDL-C, low-density lipoprotein cholesterol; MI, myocardial infarction; p; probability; PAD, peripheral artery disease; PVD, peripheral vascular disease.
Literature Review Flow Diagram for Chapter 24: Screening for the Presence of Cardiovascular Disease
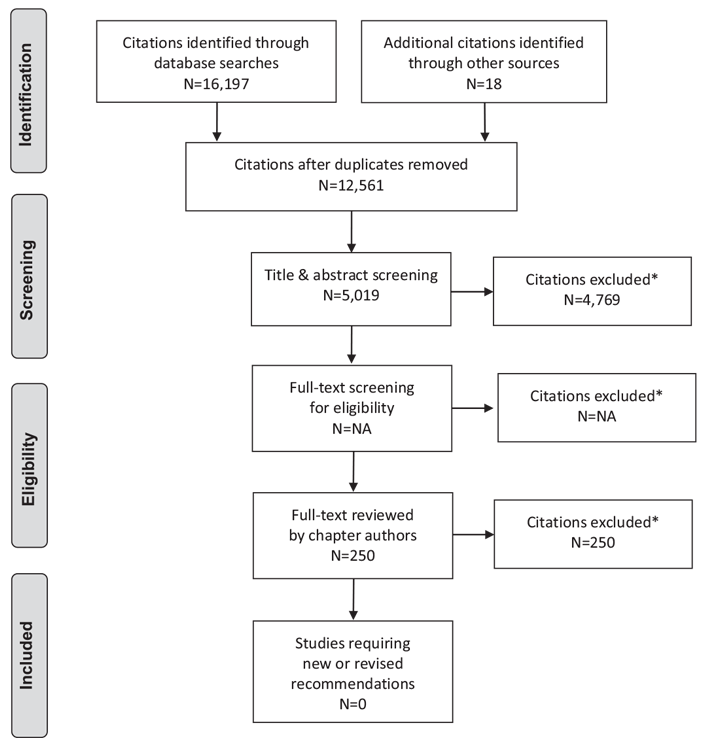
*Excluded based on: population, intervention/exposure, comparator/control or study design.
NA—not applicable.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(6): e1000097. doi:10.1371/journal.pmed1000097 (99).
For more information, visit www.prisma-statement.org.
References
- Lee WL, Cheung AM, Cape D, et al. Impact of diabetes on coronary artery disease in women and men: A meta-analysis of prospective studies. Diabetes Care 2000;23:962-8.
- Booth GL, Kapral MK, Fung K, et al. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: A population-based retrospective cohort study. Lancet 2006;368:29-36.
- Cohn PF, Fox KM, Daly C. Silentmyocardial ischemia. Circulation 2003;108:1263-77.
- Bulugahapitiya U, Siyambalapitiya S, Sithole J, et al. Is diabetes a coronary risk equivalent? Systematic review and meta-analysis. Diabet Med 2009;26:142-8.
- Van Werkhoven JM, Cademartiri F, Seitun S, et al. Diabetes: Prognostic value of CT coronary angiography-comparison with a nondiabetic population. Radiology 2010;256:83-92.
- Cortigiani L, Bigi R, Sicari R, et al. Prognostic value of pharmacological stress echocardiography in diabetic and nondiabetic patients with known or suspected coronary artery disease. J Am Coll Cardiol 2006;47:605-10.
- Raggi P, Shaw LJ, Berman DS, et al. Prognostic value of coronary artery calcium screening in subjects with and without diabetes. J Am Coll Cardiol 2004;43:1663-9.
- Young LH, Wackers FJ, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: The DIAD study: A randomized controlled trial. JAMA 2009;301:1547-55.
- Lievre MM, Moulin P, Thivolet C, et al. Detection of silent myocardial ischemia in asymptomatic patients with diabetes: Results of a randomized trial and metaanalysis assessing the effectiveness of systematic screening. Trials 2011;12:23.
- Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16.
- Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009;360:2503-15.
- Turrini F, Scarlini S, Mannucci C, et al. Does coronary Atherosclerosis Deserve to be Diagnosed earlY in Diabetic patients? The DADDY-D trial. Screening diabetic patients for unknown coronary disease. Eur J Intern Med 2015;26:407-13.
- Zellweger MJ, Hachamovitch R, Kang X, et al. Prognostic relevance of symptoms versus objective evidence of coronary artery disease in diabetic patients. Eur Heart J 2004;25:543-50.
- Rajagopalan N, Miller TD, Hodge DO, et al. Identifying high-risk asymptomatic diabetic patients who are candidates for screening stress single-photon emission computed tomography imaging. J Am Coll Cardiol 2005;45:43-9.
- Weiner DA, Ryan TJ, Parsons L, et al. Significance of silent myocardial ischemia during exercise testing in patients with diabetes mellitus: A report fromthe Coronary Artery Surgery Study (CASS) Registry. Am J Cardiol 1991;68:729-34.
- Inoguchi T, Yamashita T, Umeda F, et al. High incidence of silentmyocardial ischemia in elderly patients with non insulin-dependent diabetes mellitus. Diabetes Res Clin Pract 2000;47:37-44.
- Nesto RW, Phillips RT, Kett KG, et al. Angina and exertional myocardial ischemia in diabetic and nondiabetic patients: Assessment by exercise thallium scintigraphy. Ann Intern Med 1988;108:170-5.
- Bacci S, Villella M, Villella A, et al. Screening for silent myocardial ischaemia in type 2 diabetic patients with additional atherogenic risk factors: Applicability and accuracy of the exercise stress test. Eur J Endocrinol 2002;147:649-54.
- Wackers FJ, Young LH, Inzucchi SE, et al. Detection of silent myocardial ischemia in asymptomatic diabetic subjects: The DIAD study. Diabetes Care 2004;27:1954-61.
- Myers J, Prakash M, Froelicher V, et al. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 2002;346:793-801.
- Sorajja P, Chareonthaitawee P, Rajagopalan N, et al. Improved survival in asymptomatic diabetic patients with high-risk SPECT imaging treated with coronary artery bypass grafting. Circulation 2005;112:I311-16.
- Paillole C, Ruiz J, Juliard JM, et al. Detection of coronary artery disease in diabetic patients. Diabetologia 1995;38:726-31.
- Milan Study on Atherosclerosis and Diabetes (MiSAD) Group. Prevalence of unrecognized silent myocardial ischemia and its association with atherosclerotic risk factors in noninsulin-dependent diabetes mellitus. Am J Cardiol 1997;79:134-9.
- Faglia E, Favales F, Calia P, et al. Cardiac events in 735 type 2 diabetic patients who underwent screening for unknown asymptomatic coronary heart disease: 5-year follow-up report from the Milan Study on Atherosclerosis and Diabetes (MiSAD). Diabetes Care 2002;25:2032-6.
- Muhlestein JB, Lappe DL, Lima JA, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: The FACTOR-64 randomized clinical trial. JAMA 2014;312:2234-43.
- Faglia E, Manuela M, Antonella Q, et al. Risk reduction of cardiac events by screening of unknown asymptomatic coronary artery disease in subjects with type 2 diabetes mellitus at high cardiovascular risk: An open-label randomized pilot study. Am Heart J 2005;149:e1-6.
- Zellweger MJ, Maraun M, Osterhues HH, et al. Progression to overt or silent CAD in asymptomatic patients with diabetes mellitus at high coronary risk: Main findings of the prospective multicenter BARDOT trial with a pilot randomized treatment substudy. JACC Cardiovasc Imaging 2014;7:1001-10.
- Budoff MJ, Raggi P, Beller GA, et al. Noninvasive cardiovascular risk assessment of the asymptomatic diabetic patient: The imaging council of the American College of Cardiology. JACC Cardiovasc Imaging 2016;9:176-92.
- Elhendy A, Arruda AM, Mahoney DW, et al. Prognostic stratification of diabetic patients by exercise echocardiography. J Am Coll Cardiol 2001;37:1551-7.
- Anand DV, Lim E, Hopkins D, et al. Risk stratification in uncomplicated type 2 diabetes: Prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy. Eur Heart J 2006;27:713-21.
- Andreini D, Pontone G, Mushtaq S, et al. Prognostic value of multidetector computed tomography coronary angiography in diabetes: Excellent long-term prognosis in patients with normal coronary arteries. Diabetes Care 2013;36:1834-41.
- Poirier P, Garneau C, Bogaty P, et al. Impact of left ventricular diastolic dysfunction on maximal treadmill performance in normotensive subjects with wellcontrolled type 2 diabetes mellitus. Am J Cardiol 2000;85:473-7.
- Poirier P, Bogaty P, Garneau C, et al. Diastolic dysfunction in normotensive men with well-controlled type 2 diabetes: Importance of maneuvers in echocardiographic screening for preclinical diabetic cardiomyopathy. Diabetes Care 2001;24:5-10.
- Curtis JM, Horton ES, Bahnson J, et al. Prevalence and predictors of abnormal cardiovascular responses to exercise testing among individuals with type 2 diabetes: The Look AHEAD (Action for Health in Diabetes) study. Diabetes Care 2010;33:901-7.
- Rutter MK, McComb JM, Brady S, et al. Silent myocardial ischemia and microalbuminuria in asymptomatic subjects with non-insulin-dependent diabetes mellitus. Am J Cardiol 1999;83:27-31.
- Rutter MK, Wahid ST, McComb JM, et al. Significance of silent ischemia and microalbuminuria in predicting coronary events in asymptomatic patients with type 2 diabetes. J Am Coll Cardiol 2002;40:56-61.
- Erne P, Schoenenberger AW, ZuberM, et al. Effects of anti-ischaemic drug therapy in silent myocardial ischaemia type I: The Swiss Interventional Study on Silent Ischaemia type I (SWISSI I): A randomized, controlled pilot study. Eur Heart J 2007;28:2110-17.
- Padala SK, Ghatak A, Padala S, et al. Cardiovascular risk stratification in diabetic patients following stress single-photon emission-computed tomography myocardial perfusion imaging: The impact of achieved exercise level. J Nucl Cardiol 2014;21:1132-43.
- Peix A, Cabrera LO, Rodriguez L, et al. Cardiac outcomes 3 years after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: Value of myocardial perfusion imaging and coronary calcium score. Nucl Med Commun 2015;36:156-61.
- Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol 2004;11:171-85.
- Schinkel AF, Bax JJ, Elhendy A, et al. Long-term prognostic value of dobutamine stress echocardiography compared withmyocardial perfusion scanning in patients unable to perform exercise tests. Am J Med 2004;117:1-9.
- Bax JJ, Young LH, Frye RL, et al. Screening for coronary artery disease in patients with diabetes. Diabetes Care 2007;30:2729-36.
- van den Hoogen IJ, de Graaf MA, Roos CJ, et al. Prognostic value of coronary computed tomography angiography in diabetic patients without chest pain syndrome. J Nucl Cardiol 2016;23:24-36.
- Anand DV, Lim E, Darko D, et al. Determinants of progression of coronary artery calcification in type 2 diabetes role of glycemic control and inflammatory/ vascular calcification markers. J Am Coll Cardiol 2007;50:2218-25.
- Lundin M, Wiksten JP, Peräkylä T, et al. Distal pulse palpation: Is it reliable? World J Surg 1999;23:252–5.
- Mowlavi A, Whiteman J, Wilhelmi BJ, et al. Dorsalis pedis arterial pulse: Palpation using a bony landmark. Postgrad Med J 2002;78:746–7.
- Lehto S, Niskanen L, Suhonen M, et al. Medial artery calcification. A neglected harbinger of cardiovascular complications in non-insulin-dependent diabetes mellitus. Arterioscler Thromb Vasc Biol 1996;16:978–83.
- Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: Results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation 2004;110:738–43.
- Jude EB, Oyibo SO, Chalmers N, et al. Peripheral arterial disease in diabetic and nondiabetic patients: A comparison of severity and outcome. Diabetes Care 2001;24:1433–7.
- van der Feen C, Neijens FS, Kanters SD, et al. Angiographic distribution of lower extremity atherosclerosis in patients with and without diabetes. Diabet Med 2002;19:366–70.
- ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–72.
- Mohammedi K,WoodwardM, Hirakawa Y, et al. Microvascular and macrovascular disease and risk for major peripheral arterial disease in patients with type 2 diabetes. Diabetes Care 2016;39:1796–803.
- Adler AI, Stevens RJ, Neil A, et al. UKPDS 59: Hyperglycemia and other potentially modifiable risk factors for peripheral vascular disease in type 2 diabetes. Diabetes Care 2002;25:894–9.
- Althouse AD, Abbott JD, Forker AD, et al. Risk factors for incident peripheral arterial disease in type 2 diabetes: Results from the Bypass Angioplasty Revascularization Investigation in type 2 Diabetes (BARI 2D) Trial. Diabetes Care 2014;37:1346–52.
- Fiordaliso F, Clerici G, Maggioni S, et al. Prospective study on microangiopathy in type 2 diabetic foot ulcer. Diabetologia 2016;59:1542–8.
- Sebastianski M, Makowsky MJ, Dorgan M, et al. Paradoxically lower prevalence of peripheral arterial disease in South Asians: A systematic review and meta-analysis. Heart 2014;100:100–5.
- Mohammedi K, Woodward M, Zoungas S, et al. Absence of peripheral pulses and risk of major vascular outcomes in patients with type 2 diabetes. Diabetes Care 2016;39:2270–7.
- Criqui MH, Fronek A, Klauber MR, et al. The sensitivity, specificity, and predictive value of traditional clinical evaluation of peripheral arterial disease: Results from noninvasive testing in a defined population. Circulation 1985;71:516–22.
- Hiatt WR, Marshall JA, Baxter J, et al. Diagnostic methods for peripheral arterial disease in the San Luis Valley Diabetes Study. J Clin Epidemiol 1990;43:597–606.
- Collins TC, Suarez-Almazor M, Peterson NJ. An absent pulse is not sensitive for the early detection of peripheral arterial disease. Fam Med 2006;38:38–42.
- Silverman JJ. The incidence of palpable dorsalis and pedis and posterior tibial pulsations in soldiers; an analysis of over 1,000 infantry soldiers. Am Heart J 1946;32:82–7.
- Turkbey EB, Backlund JY, Genuth S, et al. Myocardial structure, function, and scar in patients with type 1 diabetes mellitus. Circulation 2011;124:1737–46.
- Soedamah-Muthu SS, Fuller JH, Mulnier HE, et al. High risk of cardiovascular disease in patients with type 1 diabetes in the U.K.: A cohort study using the general practice research database. Diabetes Care 2006;29:798–804.
- Schram MT, Chaturvedi N, Fuller JH, et al. Pulse pressure is associated with age and cardiovascular disease in type 1 diabetes: The Eurodiab Prospective Complications Study. J Hypertens 2003;21:2035–44.
- Caccamo G, Bonura F, Bonura F, et al. Insulin resistance and acute coronary syndrome. Atherosclerosis 2010;211:672–5.
- Krolewski AS, Kosinski EJ, Warram JH, et al. Magnitude and determinants of coronary artery disease in juvenile-onset, insulin-dependent diabetes mellitus. Am J Cardiol 1987;59:750–5.
- Libby P, Nathan DM, Abraham K, et al. Report of the National Heart, Lung, and Blood Institute-National Institute of Diabetes and Digestive and Kidney DiseasesWorking Group on cardiovascular complications of type 1 diabetes mellitus. Circulation 2005;111:3489–93.
- Deckert T, Poulsen JE, Larsen M. Prognosis of diabetics with diabetes onset before the age of thirty-one. I. Survival, causes of death, and complications. Diabetologia 1978;14:363–70.
- Pambianco G, Costacou T, Ellis D, et al. The 30-year natural history of type 1 diabetes complications: The Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes 2006;55:1463–9.
- Waden J, Forsblom C, Thorn LM, et al. A1C variability predicts incident cardiovascular events, microalbuminuria, and overt diabetic nephropathy in patients with type 1 diabetes. Diabetes 2009;58:2649–55.
- Conway B, Costacou T, Orchard T. Is glycaemia or insulin dose the stronger risk factor for coronary artery disease in type 1 diabetes? Diab Vasc Dis Res 2009;6:223–30.
- Klein BE, Klein R, McBride PE, et al. Cardiovascular disease, mortality, and retinal microvascular characteristics in type 1 diabetes: Wisconsin epidemiologic study of diabetic retinopathy. Arch Intern Med 2004;164:1917–24.
- Weis U, Turner B, Gibney J, et al. Long-term predictors of coronary artery disease and mortality in type 1 diabetes. QJM 2001;94:623–30.
- Laing SP, Swerdlow AJ, Slater SD, et al. Mortality from heart disease in a cohort of 23,000 patients with insulin-treated diabetes. Diabetologia 2003;46:760–5.
- Putaala J, Kurkinen M, Tarvos V, et al. Silent brain infarcts and leukoaraiosis in young adults with first-ever ischemic stroke. Neurology 2009;72:1823–9.
- Moss SE, Klein R, Klein BE. The 14-year incidence of lower-extremity amputations in a diabetic population. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. Diabetes Care 1999;22:951–9.
- Jonasson JM, Ye W, Sparen P, et al. Risks of nontraumatic lower-extremity amputations in patients with type 1 diabetes: A population-based cohort study in Sweden. Diabetes Care 2008;31:1536–40.
- Carter RE, Lackland DT, Cleary PA, et al. Intensive treatment of diabetes is associated with a reduced rate of peripheral arterial calcification in the diabetes control and complications trial. Diabetes Care 2007;30:2646–8.
- Olson JC, Erbey JR, Forrest KY, et al. Glycemia (or, in women, estimated glucose disposal rate) predict lower extremity arterial disease events in type 1 diabetes. Metabolism 2002;51:248–54.
- Margeirsdottir HD, Stensaeth KH, Larsen JR, et al. Early signs of atherosclerosis in diabetic children on intensive insulin treatment: A population-based study. Diabetes Care 2010;33:2043–8.
- Jarvisalo MJ, Putto-Laurila A, Jartti L, et al. Carotid artery intima-media thickness in children with type 1 diabetes. Diabetes 2002;51:493–8.
- Yamasaki Y, Kawamori R, Matsushima H, et al. Atherosclerosis in carotid artery of young IDDM patients monitored by ultrasound high-resolution B-mode imaging. Diabetes 1994;43:634–9.
- Dalla Pozza R, Bechtold S, Bonfig W, et al. Age of onset of type 1 diabetes in children and carotid intima medial thickness. J Clin Endocrinol Metab 2007;92:2053–7.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001;285:2486–97.
- Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005;353:2643–53.
- Larsen J, Brekke M, Sandvik L, et al. Silent coronary atheromatosis in type 1 diabetic patients and its relation to long-term glycemic control. Diabetes 2002;51:2637–41.
- Orchard TJ, Costacou T. When are type 1 diabetic patients at risk for cardiovascular disease? Curr Diab Rep 2010;10:48–54.
- Colhoun HM, Rubens MB, Underwood SR, et al. The effect of type 1 diabetes mellitus on the gender difference in coronary artery calcification. J Am Coll Cardiol 2000;36:2160–7.
- Laing SP, Swerdlow AJ, Slater SD, et al. The British Diabetic Association Cohort Study, II: Cause-specific mortality in patients with insulin-treated diabetes mellitus. Diabet Med 1999;16:466–71.
- Skrivarhaug T, Bangstad HJ, Stene LC, et al. Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Diabetologia 2006;49:298–305.
- Secrest AM, Becker DJ, Kelsey SF, et al. Cause-specific mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes. Diabetes 2010;59:3216–22.
- Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2010;122:e584–636.
- American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care 2011;34 Suppl 1:S11–61.
- Olson JC, Edmundowicz D, Becker DJ, et al. Coronary calcium in adults with type 1 diabetes: A stronger correlate of clinical coronary artery disease in men than in women. Diabetes 2000;49:1571–8.
- Cleary PA, Orchard TJ, Genuth S, et al. The effect of intensive glycemic treatment on coronary artery calcification in type 1 diabetic participants of the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study. Diabetes 2006;55:3556–65.
- Dabelea D, Kinney G, Snell-Bergeon JK, et al. Effect of type 1 diabetes on the gender difference in coronary artery calcification: A role for insulin resistance? The Coronary Artery Calcification in Type 1 Diabetes (CACTI) Study. Diabetes 2003;52:2833–9.
- Wolk MJ, Bailey SR, Doherty JU, et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/ SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 2014;63:380–406.
- Bauters C, Lemesle G. Screening for asymptomatic coronary artery disease in patients with diabetes mellitus: A systematic review and meta-analysis of randomized trials. BMC Cardiovasc Disord 2016;16:90.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009;6: e1000097.